Recent trends, have shown that love and prosperity have agreed. People are starting to love again; Take a look!
Black people; white people are all coming together We are putting our hands and heart together to ask ”Why is this “? “Who Is this?.” Politics , violence , and agendas have angered us; all of our races; it has damaged the system; especially our hearts!
- The assignment here in our world is to make things easy, but it is too easy to get corrupt .
With the recent trends of nationwide debate and protests over systemic racism and police violence, of course the U.S. has taken center stage!
We have a melting pot that hasn’t been stirred; there’s white who are one one side ; blacks who are on another; and the Native Americans asking “who are we?” . We are not judges..NONE can think less of none .But still ,All across the country we are having the strangest conversations with one another while avoiding the deeper ones; we need to have; diversity, human representation and economic inclusion. But how can we do these things if we we never develop the feelings involved?.We positively say our point; but with no heart and anger.
But what is the world hearing, and how are other countries making their voices heard in this debate?
France I know had recently spoken on Black inclusion in their country; Hispanics are also pushing the young not to trust anyone with information. If the world is trying to understand how to include difference we shouldn’t preach. The message should comes from our actions, our simple spaces. We got to chill our hearts and minds; that will fix our EYES judging ; what I mean is Behavior is meaningless if we don’t think less ; we got to see kindly in order to do that. The more we are in our heads the more we pull out conflicts.
What does BLM mean for public health and global health? Think about the influence of discrimination and racism on health more broadly?
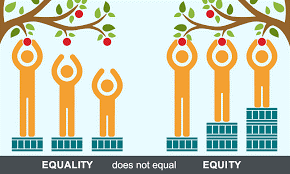
- “The Black Lives Matter movement has been an important enlightener to the pervasive problem of police and other forms of violence against the Black community. But the movement’s success also shows us the importance of decentralizing power, listening to, and taking seriously the expertise and needs of those most affected by a problem—rather than imposing”
- According to the article “Shifting power from distant, donor-country elites to local aid recipients will lead to stronger global health systems”
- They claim Global Health organizations have been “backending” different colleges; by creating unequal powers structures through offering them short contracts for two-years ; but I say when do contracts ever HAVEN’T shorted us? Why? They tie a limits on our leases,
- I will offer a better opinion in relating this movement (discrimination effecting Global health agencies) ; a lot of people have issues hiring black people; so they leave the blunt work or the work with communication ; but the work of engaging and positive thinking higher skills; they leave to other races; whites; is this correct? I offer; it’s only wrong when you never share what you know ; especially if someone asks.
I have learned through experience that granting someone else knowledge/skills/opportunities when requested by another can can heal there fears, and injustices; not just provide them a job alone.
Let’s have more opportunities in Global health work open for the Races that want to raise themselves. Our feet out hot ; but our minds are cold. We have to open up because some people will never if they never see a door . Let’s concentrate on the art of giving; and sharing; the language of Love Divine; then we can see how it works here on this planet.
- Question; is a doctor judged by the coat he where’s or his skin:
- We tend to find the right doctors based on who we are; our mirrors.
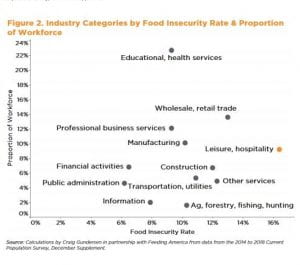
Think about the health disparities? Those which arisen because of the discrimination and inequity. How can we address these health disparities?
- The concentration of poverty inequality can lead to stress and hardship as well as other chronic and acute stressors at the individual level.
- “The institutional neglect and disinvestment in poor, segregated communities contributes to increased exposure to environmental toxins, poor quality housing and criminal victimization.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3468327/
What do health disparities mean for the African diaspora across other parts of the world? What about intersectionality, particularly for women of color? May these issues be related to the high infant mortality rate in our state of Georgia?
- For members of the African Diaspora, aka “heat adapted people“Ecological adaptations to tropical climate have been shaped the genetic structure
- “Local temperature-induced adaptive genetic changes may be one mechanism involved in hypertension and differences in salt sensitivity in them .”
What this means for diaspora, across parts of the worlds is that the have greater risk of hypertension and other diseases due to exposures of interaction to the modern world. (I.E.)They have not adapted well yet
https://www.sciencedirect.com/science/article/pii/S0959437X16301095
These Genetic differences defiantly can effect Women Of Color especially through ancestor lineage.
- African American women have 2.3 times the infant mortality rate as non-Hispanic whites.
- African American infants are 3.8 times as likely to die from complications related to low birth weight as compared to non-Hispanic white infants.
https://dph.georgia.gov/infant-mortality
Yes I beleive these issues are , because the (average), infant mortality rate (per 1,000 live births) in Georgia was highest for Black infants (11.7)
https://dph.georgia.gov/infant-mortality
CONCLUSION
- Black Lives ,are effected in all fields, both economically,systemically, physically(health) . As discussed with what “BLM” means for the global health and public health fields, Global health agencies have to speak up more for better funding ,better treatment, and better equality. As far as how it effects our health specifically, we should invitee more doctors of color into our health sector, and personalized treatments.
- African Diaspora are all trying to fit in this melting pot because they have been displaced culturally, and ancestrally, these displacements as discussed effect there health, life and well being. It all parallels directly with the same things that African Americans are facing today, (I.e hypertension, high salt intake/the topics discussed above) . All of these ultimately effect women of color, because they are largely marrying black men.


























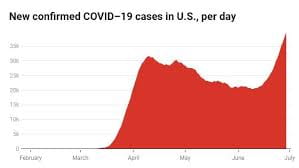
 Symptoms involving difficulty breathing, muscle and body aches, headaches, losses of taste and smell, and fatigue are just a few signs that you have likely been infected with this lethal virus. We have been told to stay at home, to quarantine with loved ones, to wear a mask in public, and to wash our hands thoroughly as safety measures in order to combat the growing number of cases every day. Public health officials, medical professionals, and
Symptoms involving difficulty breathing, muscle and body aches, headaches, losses of taste and smell, and fatigue are just a few signs that you have likely been infected with this lethal virus. We have been told to stay at home, to quarantine with loved ones, to wear a mask in public, and to wash our hands thoroughly as safety measures in order to combat the growing number of cases every day. Public health officials, medical professionals, and 
 , ensuring they are getting proper exercise and sleep, and by asking them if they need anything, within reason, that you may be able to provide. In addition to checking in on your loved ones, it is important to check in with yourself as well. Not everything lands on your shoulders and there is no reason to believe that you are responsible for other people’s actions, so make sure to take some time to free yourself from your responsibilities as well. In addition to checking in on our loved ones, important policies and programs need to be created for communities in order to combat mental health illnesses. Education and training programs need to be provided to health system leaders, first responders, and health care professionals on psychosocial issues (Pfefferbaum, 2020). Furthermore, emergency response communities need to work together to identify and develop resources that can be related to mental health triage and referrals (Pfefferbaum, 2020). Lastly, it is important to integrate mental health practices as health care workers are already overworked in their efforts to combat the disease medically (Pfefferbaum, 2020).
, ensuring they are getting proper exercise and sleep, and by asking them if they need anything, within reason, that you may be able to provide. In addition to checking in on your loved ones, it is important to check in with yourself as well. Not everything lands on your shoulders and there is no reason to believe that you are responsible for other people’s actions, so make sure to take some time to free yourself from your responsibilities as well. In addition to checking in on our loved ones, important policies and programs need to be created for communities in order to combat mental health illnesses. Education and training programs need to be provided to health system leaders, first responders, and health care professionals on psychosocial issues (Pfefferbaum, 2020). Furthermore, emergency response communities need to work together to identify and develop resources that can be related to mental health triage and referrals (Pfefferbaum, 2020). Lastly, it is important to integrate mental health practices as health care workers are already overworked in their efforts to combat the disease medically (Pfefferbaum, 2020).



 Especially in the United States, healthcare has changed from in-person visits with a healthcare practitioner to a telehealth visit. There have been many positive and negative effects that vary greatly from person to person concerning this switch. For example, many of the large health insurance companies have begun to cover telehealth visits at 100% to their subscribers with no copay, therefore benefiting the patients to use this service. A potential major obstacle to telehealth visits for some people could be internet access or computer and internet access. In contrast though, most Americans have access to a computer/mobile phone with internet capabilities. For those healthcare practitioners/offices that cannot participate in telehealth visits such as chiropractors, oncology, allergist, etc. patient care has still continued on, just with a very different look than patients are used to. The chairs in the waiting room (if the waiting room is even open) are 6 feet apart, everyone is required to wear masks, cleaning of rooms and surfaces has increased drastically, and charting has been moved to 100% digital. Some of these changes are for the better and I hope will stay implemented even after the pandemic has “ended”. The current coronavirus pandemic has made everyone aware that the United States and arguably most countries across the world, were not and are not prepared for a pandemic and the associated burdens that it places on the healthcare world and the economic world. Here is to hoping that people learn something from this pandemic and we as a whole world are better prepared for the next one when it comes around.
Especially in the United States, healthcare has changed from in-person visits with a healthcare practitioner to a telehealth visit. There have been many positive and negative effects that vary greatly from person to person concerning this switch. For example, many of the large health insurance companies have begun to cover telehealth visits at 100% to their subscribers with no copay, therefore benefiting the patients to use this service. A potential major obstacle to telehealth visits for some people could be internet access or computer and internet access. In contrast though, most Americans have access to a computer/mobile phone with internet capabilities. For those healthcare practitioners/offices that cannot participate in telehealth visits such as chiropractors, oncology, allergist, etc. patient care has still continued on, just with a very different look than patients are used to. The chairs in the waiting room (if the waiting room is even open) are 6 feet apart, everyone is required to wear masks, cleaning of rooms and surfaces has increased drastically, and charting has been moved to 100% digital. Some of these changes are for the better and I hope will stay implemented even after the pandemic has “ended”. The current coronavirus pandemic has made everyone aware that the United States and arguably most countries across the world, were not and are not prepared for a pandemic and the associated burdens that it places on the healthcare world and the economic world. Here is to hoping that people learn something from this pandemic and we as a whole world are better prepared for the next one when it comes around.