We are currently in a period of rapid technology growth, which some have termed the “fourth industrial revolution,” and new innovative technologies are expected to benefit health and healthcare greatly. As more people across globe, including developing nations, gain access to technology, the possible applications of such tech in the health field widens. Many advanced technologies are too expensive, having little effect on health crises in areas where high-tech healthcare isn’t available, so developing ways technology can provide lower cost solutions to billions of people in less developed countries is necessary.
Many health care systems are looking into telemedicine, but there are also other ways new technologies are being employed and evaluated as possible modes of help for health officials in such countries. The following examples highlight how technologies such as, robotics/drones, mobile phones, 3D printers, and artificial intelligence can also make strides in increasing the access and effectiveness of health care where there are limited resources.
Technological Innovations being used in Developing nations:
Drone Delivery System in Rwanda:
Rwanda, like many less developed countries, is plagued by bad road infrastructure, and during the rainy season it only worsens, with many roads becoming impassable by cars and motorbikes. This transportation issue coupled with Rwanda’s high prevalence of mothers dying during childbirth due to blood loss, were the main reasons for the launch of Zipline, a California based company focused on delivering medical supplies to such areas.
Many hospitals and health centers are not able to stockpile large amounts of blood because of the short shelf life and storage requirements. When emergency blood is needed at a hospital it can take up to 5 hours, in many instances resulting in the death of the patient in need. By using drones to deliver blood, a 50 km distance, which takes over an hour by car, can arrive in less than 15 minutes.
How does it work?
When a hospital needs emergency blood, a request is sent via SMS, phone call, or website. The blood is then loaded with a parachute into the drone by the storage facility, and a smartphone application provides a preflight checklist to follow, including requesting flight clearance from the Rwandan aviation authority. A few minutes before the drone arrives at the hospital, staff are alerted by an automated text to go outside and prepare for the drop.
Though the process has shown many successes and is an impressive technology, there are many limitations and concerns. The technology is expensive and without the current subsidizes by the Rwandan government, drone use may not be cost effective; but arguments against this focus on the effect it would have on minimizing wasted blood due to expiration, paying for itself in the long run. In 2018, hospitals that used Zipline reported no waste.
Another issue is the necessity to share airspace, needing new legislation and trust by a country’s government, which many are skeptical or uncomfortable with drones. Until the drones can hold larger quantities of blood, they are only useful in emergency deliveries. The project plans to expand to deliver medicines and vaccines and move drone assembly from the U.S. to Rwanda.
mTrac in Uganda:
In 2015 Uganda’s mobile phone usage grew to about 65%, creating new opportunities for healthcare workers and patients to improve access to “real-time” information, identify disease outbreaks, and strengthen engagement and accountability. MTrac was launched in 2009 by the Foundation for Innovative New Diagnostics and was made country wide in 2011 with the help of UNICEF. The mTrac services include the timely communication and response of healthcare workers and local governments through weekly reporting and conduction of polls and surveys able to reach all health facilities across Uganda at a low cost.
Health workers use their own basic cellphones to submit surveillance data weekly, medicine stockpile information, maternal and neonatal deaths, typhoid cases, etc., and when a “threshold” is met an alert is sent to the district health management teams for a quick response. It also includes an anonymous toll-free text hotline for Ugandans to place complaints, such as health service problems.
How has it helped?
By 2016 62,000 health workers and 4,431 health facilities were registered in the database and weekly reporting increased with 80% of facilities completing reports. Client satisfaction increased from 46% to 68% over 5 years and increasing accountability of worker absenteeism and medical supply theft. Some challenges that have arose are workers feeling “overwhelmed” because they cannot respond to everything, budget gaps, and network interferences. [case study article].
3D printing in Haiti:
The 2010 earthquake in Haiti resulted in over 100,000 deaths and the destruction of over 60% of their healthcare facilities [3dprint]. Due to the issues of transportation networks becoming congested by many different crisis relief organizations and such organizations occasional deployment of unnecessary equipment, a 3D printer pilot program, 3DforHealth, was implemented in Haiti to try and reduce such strains on resources and allow for a quicker, in country response to medical material needs.
The program helped aide in “rapid and cost effective on demand production of much needed medical instruments” [3dprint], as well as manufacture broken and missing parts of existing equipment. After interviewing medical personnel after the earthquake ended, the implementation team and local community members developed an umbilical cord clamp. The program proved to reduce the dependency on time sensitive services, and its success led to its absorption by Field Ready, a larger program for disaster response. More uses of 3D printing for health are outlined here.
AI and Malaria:
IBM Research Africa and the University of Oxford have begun using artificial intelligence to help in the decision making of officials and “explore more effective malaria policy interventions.” Interventions such as bed nets, insecticides, and repellents are known to be effective in malaria control, but with decreasing budgets is can be difficult for public health officials and policy makers to choose where to focus the money. Through the use of these AI algorithms and publicly available research and models, like OpenMalaria, officials can determine the most effective strategies for specific locations, as well as explore “what if” scenarios to assess future needs.
Through computational experiments of a 5-year intervention simulation of a region in Western Kenya, they demonstrated how AI can determine the best performing interventions in the future. While a 2017 study reported insecticide-treated bed nets were consistently the most effective across locations, these simulated scenarios showed that in Western Kenyan regions it may be more cost effective to do indoor spraying for a small portion of households rather than large scale deployment of insecticide-treated nets. Read more about AI and Malaria here.
These programs serve as examples of how new technological initiatives could improve health in developing countries and could be implemented in similar communities. There are many ways technology can help that are not mentioned including improving health education and training, clean water and sanitation, and sustainability and access to health services. Technological innovations not only can help the health field directly in low resource rural areas, but also in other fields that tend to affect health, such as agriculture, economic improvement, and transportation. There are a lot of current initiatives focusing on the needs of wealthy countries, so more inexpensive technology designed for the world’s poorest needs to be developed to improve health globally.



















:max_bytes(150000):strip_icc():format(webp)/definition-of-mental-illness-4587855-v1-cd7f9f37c61c49099ac8ede282db1e73.png)
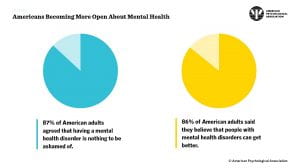
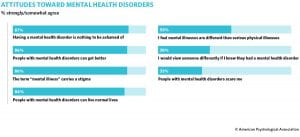
 countries, amplifying the lack of attention these illnesses receive. In 2001, it was abundantly clear that mental health illnesses were increasing in number and it was becoming imperative for people to acknowledge the severity of this issue. Unfortunately, the warnings and suggestions highlighted in the 2001 reports were not heeded and the abundance of these issues only grew. In 2017, a report from ourworldindata.org estimated that there were 792 million people living with a mental health illness. Just 16 years after the news release from WHO, there was a massive increase in the abundance of these diseases. Now, healthcare systems are taking notice, but these issues are not as easily fixed as they may seem to be.
countries, amplifying the lack of attention these illnesses receive. In 2001, it was abundantly clear that mental health illnesses were increasing in number and it was becoming imperative for people to acknowledge the severity of this issue. Unfortunately, the warnings and suggestions highlighted in the 2001 reports were not heeded and the abundance of these issues only grew. In 2017, a report from ourworldindata.org estimated that there were 792 million people living with a mental health illness. Just 16 years after the news release from WHO, there was a massive increase in the abundance of these diseases. Now, healthcare systems are taking notice, but these issues are not as easily fixed as they may seem to be.  surrounding this particular issue is extensive and is providing barriers that interfere with the quality of care that patients who suffer from these illnesses receive. Many people often stereotype those who have mental illnesses as incompetent, weak, and dangerous. These stereotypes all contribute to how the community treats those who are struggling. Although some are more explicit with their views on mental health illnesses, there are many medical providers who may not realize they are treating these patients with stereotyping attitudes. According to a research study that evaluated the impact of explicit and implicit biases of mental health illness held by medical providers, it was found that there is a mixture of both positive and negative views that essentially contribute towards the care provided. In some cases, providers feel more empathetic towards these populations which often results in very intentional methods of care for these patients. In other cases, implicit biases may creep behind the surface in which a provider may write off the patient’s symptoms. Not only do provider biases create a barrier in treatment options for these patients, but the explicit biases of the general
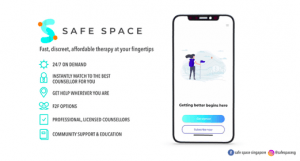
surrounding this particular issue is extensive and is providing barriers that interfere with the quality of care that patients who suffer from these illnesses receive. Many people often stereotype those who have mental illnesses as incompetent, weak, and dangerous. These stereotypes all contribute to how the community treats those who are struggling. Although some are more explicit with their views on mental health illnesses, there are many medical providers who may not realize they are treating these patients with stereotyping attitudes. According to a research study that evaluated the impact of explicit and implicit biases of mental health illness held by medical providers, it was found that there is a mixture of both positive and negative views that essentially contribute towards the care provided. In some cases, providers feel more empathetic towards these populations which often results in very intentional methods of care for these patients. In other cases, implicit biases may creep behind the surface in which a provider may write off the patient’s symptoms. Not only do provider biases create a barrier in treatment options for these patients, but the explicit biases of the general  population contribute greatly to those who need to seek care. Patients of mental health illnesses are often afraid of the
population contribute greatly to those who need to seek care. Patients of mental health illnesses are often afraid of the 
 especially
especially