Although our healthcare system has come a long way, there are still disparities in mental health treatment among racial/ethnic minority populations in the United States. The modern mental health care system has struggled with inequality based on socioeconomic status, race, and ethnicity. Those considered to be ethnic minority groups are faced with a number of barriers that prevent them from actively participating in treatment for mental disorders/illness. Due to the negative connotations that surround them, mental disorders/illnesses are commonly overlooked and go untreated. To add, minority groups in the lower socioeconomic status frequently have poor physical health, which adds to the vulnerability to mental illness. Those in this group often have a lack of options for affordable treatment and accessible resources. Both stigma and various cultural beliefs and attitudes generate discrimination and social distancing behaviors towards those suffering from mental illness. This often results in underutilization, underrepresentation, and discrepancy of mental health services amongst minority populations.

In some cases of serious mental illnesses, a person’s ability to carry out essential aspects of daily life can be interrupted. Severity ranges among the several types of mental illnesses, however, the most common disorders are the ones we have discussed when we bring up mental health, those are depression, substance abuse, bipolar disorders, anxiety disorders, panic attacks, phobias, eating disorders, schizophrenia, and dementia. Causes of mental illness have been studied and can range from inherited traits/genetics to environmental factors, biological factors, social/cultural factors, and even life experiences, for example, excessive stress. Left untreated mental illnesses can cause physical and behavioral health problems. However, due to various negative connotations surrounding mental disorders and illness, people will often attempt to ignore, reject, or self-medicate the condition in a state of denial. Minority populations suffering from mental health disorders are also less likely to utilize access to mental health services or seek out a mental health professional, and also receive poor quality mental health care.

Many studies in the past exploring attitudes about mental health services have unfortunately used either too small or large nonrepresentative samples, making it difficult to find the relation between attitudes and service use. Understanding the demographics of the population of those willing to seek mental health care can guide targeted public health interventions to increase treatment effectiveness. The situation of negative stigmas toward mental health treatment can persist beyond the starting of the treatment. It has been studied that certain demographics experience more uncomfortableness speaking with a mental health professional and also do not trust the treatment as they believe it will be ineffective. These same demographics have been observed to exhibit higher treatment dropout rates as well.
Recent studies have shown that specifically, both African Americans and minorities underutilize the professional mental health services available to them, this is probably driven by the uncertainty of the effectiveness of the health care system this results in viewing the mental health service as a place to be fearfully avoided rather than a provider of health service. Using data from questions assessing comfort, probability, and embarrassment when it comes to help-seeking for mental illness was used in a contemporaneous population-based survey. The data from the US National Comorbidity Survey and the Ontario Health Survey were analyzed to examine the correlation of a derived negative attitude. In both America and Canada, negative attitudes towards seeking help for mental illness was prevalent. Negative attitudes towards seeking help were highest among youth in low socioeconomic class, less-educated men, and single people in Ontario and the United States. Also, in both countries, not seeking treatment in the past, antisocial personality disorder and substance abuse was associated with even greater negative attitudes.
In class, we have discussed that there is evidence that different ethnic /cultural minority groups, in one case Black people, are treated differently in hospital settings. For example, they could be prescribed drugs at different rates for the same illnesses as whites. This does translate into mental health. In one case we do find that, among students in similar positions, those who are White are more likely to be diagnosed and to be prescribed medication for ADHD, even if they are displaying the same clinical needs. ADHD diagnosis for African Americans, Hispanics, and children of other races/ethnicities were respectively (95% CI) 69%, 50%, and 46% lower than it was for their white counterparts. This trend was observed in multiple nationally representative datasets. This racial disparity was observed to emerges as early as kindergarten, where black children in the United States were 70% less likely to be diagnosed with ADHD than other similarly situated White children. In this same study, Hispanic children initially seemed to be underdiagnosed for ADHD, however, this disparity became statistically nonsignificant after a controlling factor for whether a language other than English was primarily spoken in the home. Using analysis by kindergarten teachers on classroom behaviors, neither Black nor Hispanic children showed no different rate of ADHD‐related behaviors than Whites.![AJPHThinkTank on Twitter: "Wallace et. al.: Exposure to racial discrimination has incremental negative long-term effects on the mental health of ethnic minority people in the UK. [https://t.co/PCqYUMAt1l] @PublicHealth @AMJPublicHealth #PublicHealth ...](https://pbs.twimg.com/media/DrLwuXyX4AAU0Tx.jpg)
So what does this research tell us? That relying simply on the present mental healthcare systems without considering the unique barriers to quality care that apply to racial/ethnic minorities is unlikely to affect the pattern of disparities observed. It is safe to say those populations reluctant to visit the clinic for depression care may have correctly anticipated the limited quality available.
The mental health system’s race-blind approach to both treatment and research is largely the reason that the racial/ethnic minorities are underrepresented in psychological research. Challenges for practitioners and researchers should focus on some long-neglected areas, such as not assuming all ethnic/racial minorities have similar experiences, adversities, cultural backgrounds, and reactions that their reaction to treatment and interventions will vary. The mental health disparity comes in the form of both who has access to mental health treatment, and who feels represented and understood in published research articles and studies, the assumed normative default is often white experiences and behaviors.






 VR is one of the new and upcoming technology items that has the creative ability to be used in public health in all areas around the world. VR is different than AR (Augmented Reality) though. According to Mitchell in 2020, AR enhances the real world as it already exists, though graphical overlays and does not create a fully immersive experience. To learn more about the basic information about VR, click
VR is one of the new and upcoming technology items that has the creative ability to be used in public health in all areas around the world. VR is different than AR (Augmented Reality) though. According to Mitchell in 2020, AR enhances the real world as it already exists, though graphical overlays and does not create a fully immersive experience. To learn more about the basic information about VR, click  I know from personal experience that unless something is experienced in person, the full effect of an image will not be grasped. For example, the picture on the left is a really cool picture and you can tell that is is probably taken in a city, but the viewer has no idea or frame of reference for how tall those buildings actually are. But VR can change this! With a headset on, a person will be able to look up and get a better idea and feeling of just how massive and tall those buildings are in comparison to themselves. On the flip side, VR will also be able to educate people on how bad something is. For example, a picture will attempt to show how bad a trash covered island is, how polluted our waters are, how crowded slums in a third world county are, etc. but many people will not totally grasp the message that is trying to be sent. VR has the ability to fully immerse someone into these difficult areas and inspire people to change and get involved.
I know from personal experience that unless something is experienced in person, the full effect of an image will not be grasped. For example, the picture on the left is a really cool picture and you can tell that is is probably taken in a city, but the viewer has no idea or frame of reference for how tall those buildings actually are. But VR can change this! With a headset on, a person will be able to look up and get a better idea and feeling of just how massive and tall those buildings are in comparison to themselves. On the flip side, VR will also be able to educate people on how bad something is. For example, a picture will attempt to show how bad a trash covered island is, how polluted our waters are, how crowded slums in a third world county are, etc. but many people will not totally grasp the message that is trying to be sent. VR has the ability to fully immerse someone into these difficult areas and inspire people to change and get involved. 

 Most of the connotations associated with it throughout the years have been extremely negative. Not that long ago, people who suffered from any mental illness were sent to an asylum, hidden away from the world by their family, etc. The negative stigma that surrounds mental illness has changed since the days of leaving people locked away in mental asylums, but it has not changed that much. People today are still not receiving the professional help they need, looked down upon, let go from jobs, lose friends and family’s support, etc. But more than anything else, people with mental illnesses need support from those who are trained to help them, and those who love and care for them. For many people all over the world, cost is a major barrier to receiving the help that they deserve and need.
Most of the connotations associated with it throughout the years have been extremely negative. Not that long ago, people who suffered from any mental illness were sent to an asylum, hidden away from the world by their family, etc. The negative stigma that surrounds mental illness has changed since the days of leaving people locked away in mental asylums, but it has not changed that much. People today are still not receiving the professional help they need, looked down upon, let go from jobs, lose friends and family’s support, etc. But more than anything else, people with mental illnesses need support from those who are trained to help them, and those who love and care for them. For many people all over the world, cost is a major barrier to receiving the help that they deserve and need. 




 Therefore, it is sensitive to the constant changes in the environment and tries to match the most pertinent needs in a given community. This is evident when reviewing policies and medical techniques that were valid twenty years ago and realizing that they have been replaced a few times over. As newer diagnoses and worsening epidemics become more prevalent, the public health sector reacts by implementing new research, new medical advancements, and new programs in an attempt to restore balance. However, in a world that is changing at a lightning fast pace, it can be difficult to maintain efforts necessary to bear the weight of necessary interventions placed for the population at risk. Technology helps to provide an opportunity to maintain the stability of health in the population while also creating solutions to issues that did not have a prior solution identified. Medical innovations, research, health information systems, and more sectors of
Therefore, it is sensitive to the constant changes in the environment and tries to match the most pertinent needs in a given community. This is evident when reviewing policies and medical techniques that were valid twenty years ago and realizing that they have been replaced a few times over. As newer diagnoses and worsening epidemics become more prevalent, the public health sector reacts by implementing new research, new medical advancements, and new programs in an attempt to restore balance. However, in a world that is changing at a lightning fast pace, it can be difficult to maintain efforts necessary to bear the weight of necessary interventions placed for the population at risk. Technology helps to provide an opportunity to maintain the stability of health in the population while also creating solutions to issues that did not have a prior solution identified. Medical innovations, research, health information systems, and more sectors of  through Telehealth networks, patient portals, and other online accessible options. Through these online platforms, patients have been able to discuss any concerns they are having with their provider without the hassle of physically presenting to the office building or hospital. This advancement has created more efficient health methods in which patients and providers have the opportunity to discuss any issues or worries without the pressure and time constraint. Telehealth methods have also been proven to reduce the cost of health care for some patients as these visits often cost $40-$50 vs the $136-$176 in-person care can average (Yamamoto, 2014).
through Telehealth networks, patient portals, and other online accessible options. Through these online platforms, patients have been able to discuss any concerns they are having with their provider without the hassle of physically presenting to the office building or hospital. This advancement has created more efficient health methods in which patients and providers have the opportunity to discuss any issues or worries without the pressure and time constraint. Telehealth methods have also been proven to reduce the cost of health care for some patients as these visits often cost $40-$50 vs the $136-$176 in-person care can average (Yamamoto, 2014). 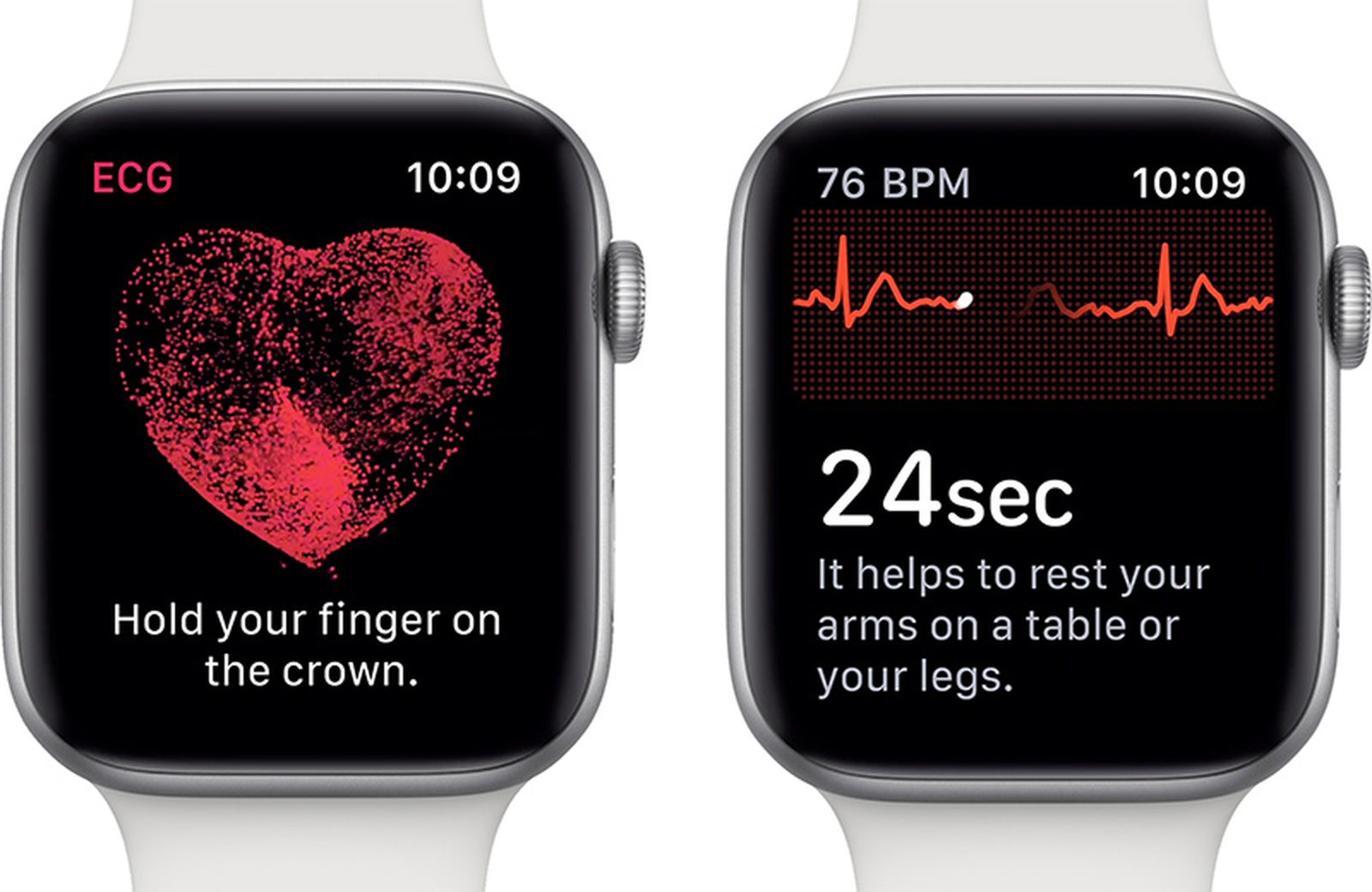 Furthermore, technological advancements in medicine have not only assisted professionals in the medical community, but have also improved patient’s lives. As devices, such as Apple Watches and Fitbits, are created to track fitness goals, there are
Furthermore, technological advancements in medicine have not only assisted professionals in the medical community, but have also improved patient’s lives. As devices, such as Apple Watches and Fitbits, are created to track fitness goals, there are 







 world. But technology has the ability to change more than just healthcare practices. The advances in technology can also change the way people farm, travel between areas that previously have been inaccessible, and many other ways that have the potential to drastically change lives.
world. But technology has the ability to change more than just healthcare practices. The advances in technology can also change the way people farm, travel between areas that previously have been inaccessible, and many other ways that have the potential to drastically change lives. Another article by Time (find it
Another article by Time (find it 