 Over the past two decades, South Korean pop culture has grown in prominence to become a significant driver of global culture. Whether you have listened to K-pop on your local radio station (BTS, Black Pink, IU, Crush, and LeeHi are a few of my favorites), watched a K-drama on Netflix (too many good ones to name them all here), purchased a Korean beauty product(e.g., sheet masks), or tried bibimpap (비빔밥) at a local Korean restaurant, you have likely been exposed to an aspect of Korean culture. Globally, many have become acquainted with the names of K-pop band members–you may know a few–or learned the ten step Korean skincare routine. However, very few are familiar with South Korea’s healthcare system, which recently received international recognition for it’s innovative and rapid response to the SARS-CoV-2 (COVID-19) pandemic. Could the influence of South Korea expand to include healthcare?
Over the past two decades, South Korean pop culture has grown in prominence to become a significant driver of global culture. Whether you have listened to K-pop on your local radio station (BTS, Black Pink, IU, Crush, and LeeHi are a few of my favorites), watched a K-drama on Netflix (too many good ones to name them all here), purchased a Korean beauty product(e.g., sheet masks), or tried bibimpap (비빔밥) at a local Korean restaurant, you have likely been exposed to an aspect of Korean culture. Globally, many have become acquainted with the names of K-pop band members–you may know a few–or learned the ten step Korean skincare routine. However, very few are familiar with South Korea’s healthcare system, which recently received international recognition for it’s innovative and rapid response to the SARS-CoV-2 (COVID-19) pandemic. Could the influence of South Korea expand to include healthcare?
South Korea’s Healthcare System: An Overview
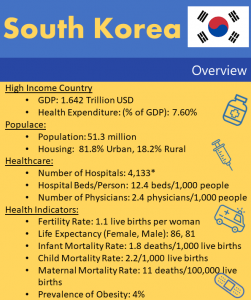
The Republic of Korea (commonly referred to as South Korea, which I will refer to as S. Korea moving forward) has a population of 51.3 million people–approximately the population of Texas and California combined–the 28th largest population in the world and 12th largest economy. As you can imagine, providing healthcare to this many people is not any easy task. However, over the span of 12 years, from 1977 to 1988, S. Korea moved from private voluntary health insurance to government-mandated healthcare. The S. Korean Healthcare System has 3 parts– the National Health Insurance Program (NHI), the Medical Aid Program, and the Long-term Care Insurance Program.
Financing Healthcare
Universal healthcare is provided to all citizens through the single-payer, National Health Insurance Corporation which is under the Ministry of Health and Wellness. It is financed through a combination of payroll  taxes, government subsidies, outside contributions, and tobacco surcharges. An average of 5.06% is deducted out of an employee’s monthly income, split between the employee and the employer to pay for health insurance. For example if you make $3,000 per month, $151.80 would go toward national health insurance.
taxes, government subsidies, outside contributions, and tobacco surcharges. An average of 5.06% is deducted out of an employee’s monthly income, split between the employee and the employer to pay for health insurance. For example if you make $3,000 per month, $151.80 would go toward national health insurance.  You would pay $75.90 and your employer would pay the other $75.90. Contributions from individuals who are self-employed are based on income and family demographics. Low-income families are exempted from monthly contributions to the health system. Tobacco surcharges provide approximately 6% of funding and the national government around 14% of funding. In 2018, S. Korea spent 7.6% of GDP on healthcare.
You would pay $75.90 and your employer would pay the other $75.90. Contributions from individuals who are self-employed are based on income and family demographics. Low-income families are exempted from monthly contributions to the health system. Tobacco surcharges provide approximately 6% of funding and the national government around 14% of funding. In 2018, S. Korea spent 7.6% of GDP on healthcare.
Coverage for Low-Income or Vulnerable Populations
The Medical Aid Program bridges health gaps affecting lower-income Koreans. The program is a  supplement for high need Koreans that are unable to contribute to the National Health Insurance. The program is jointly funded by central and local governments. The Ministry of Health sets and annually modifies the criteria for beneficiaries while local governments select the beneficiaries based on that criteria.
supplement for high need Koreans that are unable to contribute to the National Health Insurance. The program is jointly funded by central and local governments. The Ministry of Health sets and annually modifies the criteria for beneficiaries while local governments select the beneficiaries based on that criteria.
Role of Private & Public Sector
In 2018, NHI covered 97.2% of the population and the Medical Aid Program covered 2.8%. (Reference)
Koreans are free to choose their doctors and hospitals. However, most of the country’s doctors are in 
NHI relies on cost-sharing with patients, with out-of-pocket costs making up 34% of health-care expenditures, compared with an Organization for Economic Co-operation and Development (OECD) average of 20%. Inpatient care is subject to a 20% co-payment, while in outpatient care the co-payment ranges from 30% to 60% depending on the provider. For people with a low income, the Medical Aid Program covers both the insurance premium as well as co-payments. (Reference)
The government maintains ceilings on co-payments, but patients are often required to pay the full cost for services not included in the NHI benefits package, leading most people to sign up for supplemental, private insurance plans. This has resulted in unequal access to care.
private insurance plans. This has resulted in unequal access to care.
Private health insurance plans play both supplementary and complementary roles to the NHI plan. Approximately, 86.9% of South Korean households have private insurance. In 2017 the average premium for private health insurance was 287 000 won (USD 263).
If you are interested in reading more about S. Korea’s Healthcare System, these two articles will allow you to take a closer look (article 1 and article 2).
Now that you have a basic overview of the S. Korean healthcare system, do you have any thoughts about whether S. Korea should influence the U.S. healthcare system? Is S. Korean healthcare going to become apart of the Korean wave? Still not, sure? Hopefully, I will help you decide by describing the strengths and weaknesses of the S. Korean and U.S. healthcare systems.
Comparing U.S. Healthcare to S. Korea Healthcare
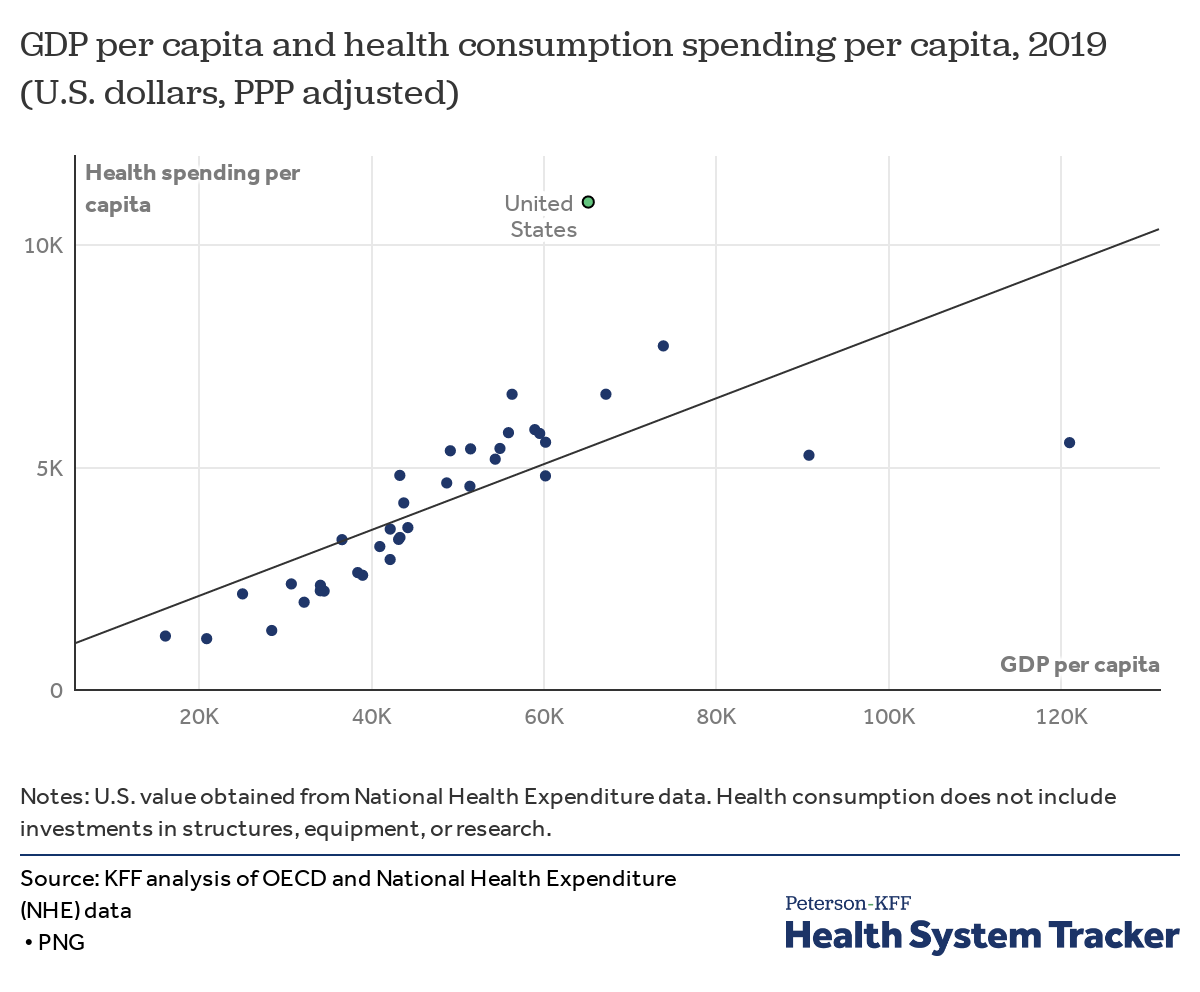
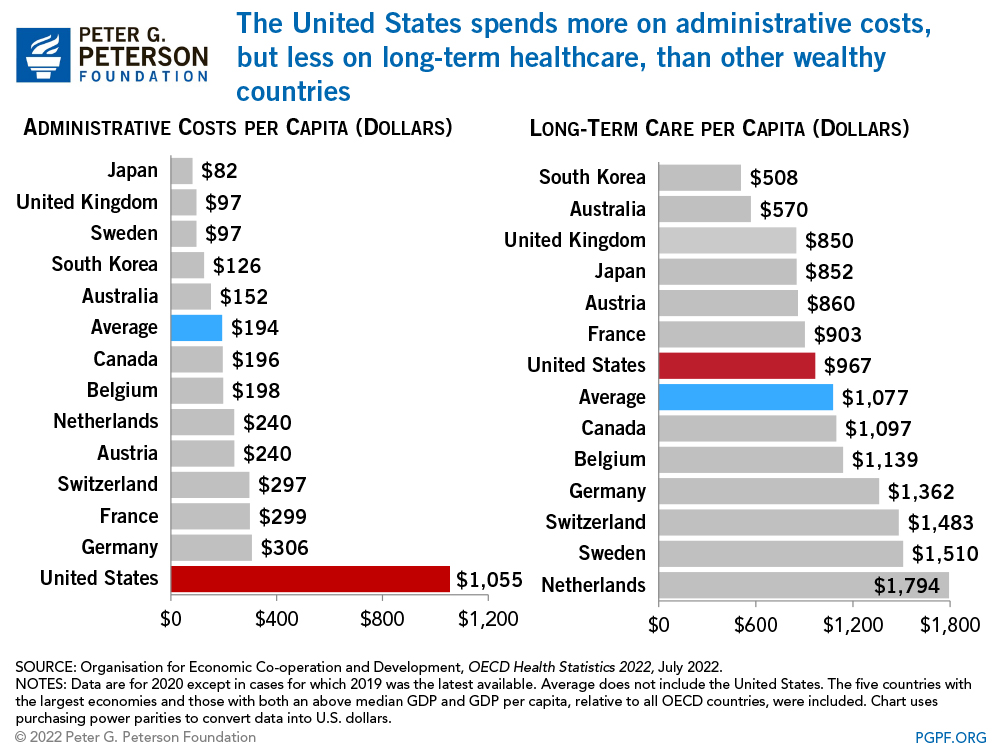
One major strength of S. Korea’s healthcare system is it’s focus on ensuring healthcare as a right for all of it’s citizens, including a program to cover low-income families. While covering every citizen, S. Korea’s healthcare spending totals less than 8% of GDP, compared with over 18% for America. S. Korea pays less than a third per capita for healthcare ($2,543) as does the United States ($11,100). With pharmaceutical prices controlled by the government, drug costs per capita total less than half America’s $1,000. Korea entered the COVID-19 pandemic with nearly four times the hospital beds per population (12.4 beds/1,000 population) as the United States (2.8 beds/1,000 population), allowing for additional capacity for COVID-19 cases. In comparison, in 2019, the U.S. closed a record number of 19 rural hospitals.

Despite these strengths, S. Korea’s healthcare system does have several weaknesses. First, most healthcare providers, specialists, and hospitals are located in urban areas of the country, specifically Seoul, making it difficult for urban populations to access treatment on a regular basis and seek care from specialist. Secondly, S. Korea does not have a strong primary care system. As Korea’s population shifts to an aging population, the healthcare system will need to strengthen it’s primary care system to prevent and manage chronic conditions. Lastly, while the government manages NHI, there is no particular focus on ensuring quality of care. Officials should ensure policies and procedures are in place to improve the quality of care throughout the country. (Reference)
















 With out-of-pocket payments making up a significant chunk of health care financing in low- and middle-income countries, identifying creative ways to cover the cost is imperative. According to a
With out-of-pocket payments making up a significant chunk of health care financing in low- and middle-income countries, identifying creative ways to cover the cost is imperative. According to a 












