Stigmas in Black Communities towards Mental Health
In black communities, there are many barriers to the lack of mental health treatment. These barriers include lack of access to care, transportation issues, lack of trust for the providers, and stigmas that are associated with mental illness. There is a prevalence of mental health issues within the black communities. Some of the disorders that are plaguing the black communities are depression, post-traumatic stress disorders, bipolar disorders, behavioral and emotional disorders, and schizophrenia to name a few. These disorders are present in other communities with a more acceptable approach in getting treated for mental health issues. Individuals in the Black communities may be more likely to deny treatment due to perceptions that have been developed within the black culture in regard to mental health. The impact of this is creating an unhealthy environment and increasing the disparities when compared to other cultures. The beliefs about mental health in the black communities are formed by cultural traditions, through experience, formal education, and stories that are shared by family and friends. Too often family members share stories of that crazy uncle are aunt that was admitted to the hospital which results in younger people adopting the behavior that someone with mental illness cannot function in society. Also, in the black communities, there are associations of someone who has a mental illness is violent. This adopted behavior will have people who commit crimes as having some level of mental illness. This stigma that has developed within the black communities is creating an environment that will only give birth to negative health outcomes. Research has indicated that black Americans underutilized voluntary mental services as a result of the negative consequences that are associated with seeking psychological help. the social pressure against psychological help-seeking and perceived difficulties associated with getting professional help ( cultural mistrust and microaggressions in therapy) It is obvious that there are disparities in regard to mental health treatment with only 1 in 3 Black Americans who could benefit from treatment receive it and lack of access to culturally competent care. These disparities will continue to exist if we do not change the community stigmas. The stigmas that we have to overcome are that depression is a personal weakness, mental illness by many people is associated with shame and embarrassment as well as many believed that since they have survived so much adversity, they’re strong and no one has the right to tell them that something is wrong with them. There need to be more intervention approaches to address this issue. There need to be more education and available resources available for the black communities. There needs to more community engagement from stakeholders as well as state and federal initiatives that are focus on programs that will increase the level of understanding of what mental health is and that it is ok to seek treatment for mental health issues.
often family members share stories of that crazy uncle are aunt that was admitted to the hospital which results in younger people adopting the behavior that someone with mental illness cannot function in society. Also, in the black communities, there are associations of someone who has a mental illness is violent. This adopted behavior will have people who commit crimes as having some level of mental illness. This stigma that has developed within the black communities is creating an environment that will only give birth to negative health outcomes. Research has indicated that black Americans underutilized voluntary mental services as a result of the negative consequences that are associated with seeking psychological help. the social pressure against psychological help-seeking and perceived difficulties associated with getting professional help ( cultural mistrust and microaggressions in therapy) It is obvious that there are disparities in regard to mental health treatment with only 1 in 3 Black Americans who could benefit from treatment receive it and lack of access to culturally competent care. These disparities will continue to exist if we do not change the community stigmas. The stigmas that we have to overcome are that depression is a personal weakness, mental illness by many people is associated with shame and embarrassment as well as many believed that since they have survived so much adversity, they’re strong and no one has the right to tell them that something is wrong with them. There need to be more intervention approaches to address this issue. There need to be more education and available resources available for the black communities. There needs to more community engagement from stakeholders as well as state and federal initiatives that are focus on programs that will increase the level of understanding of what mental health is and that it is ok to seek treatment for mental health issues.
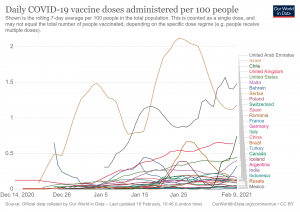
Until we are able to increase community awareness and get people comfortable with identifying that may have signs and symptoms of some form of mental illness, there will be a continued rise in mortality rates as a result of suicides and violent crimes. With the current epidemic (COVID-19) the impact of mental illness due to this virus will leave its mark on society as a whole but will have an even greater impact on Black Americans who have stigmas about mental health and treatment. the way society views mental health, or the way individuals view their issues contributes to the decision-making process in taking steps toward getting treated. to often people in the black communities will allow the stigmas to caused them not to get the treatment needed until it becomes incapacitating. One way that many blacks have been condition to believe is that mental illness is bad spirits that the only way to treat this will be to turn to the church and have the pastor pray with you to release the demons that you possess. This is another way of not wanting to accept that mental health and people who suffer from it is part of life and in order for stigmas to be removed, it’s going to take time to change a cultural behavior that has been implanted within the fabric of that community. we must not be blind to the realities that we are challenged with and collectively across cultures, it will have to be a unified effort to shift the paradigms behaviors among Black Americans so that there is equity when it comes to mental health.
References
DeFreitas, S. C., Crone, T., DeLeon, M., & Ajayi, A. (2018). Perceived and personal mental health stigma in Latino and African American college students. Frontiers in public health, 6, 49.
Fripp, J. A., & Carlson, R. G. (2017). Exploring the influence of attitude and stigma on participation of African American and Latino populations in mental health services. Journal of Multicultural Counseling and Development, 45(2), 80-94
Taylor, R. E., & Kuo, B. C. (2019). Black American psychological help-seeking intention: An integrated literature review with recommendations for clinical practice. Journal of Psychotherapy Integration, 29(4), 325.










 China has risen to global stardom in the last few decades. Its economy is increasing in capacity and is estimated to surpass the US and be the
China has risen to global stardom in the last few decades. Its economy is increasing in capacity and is estimated to surpass the US and be the 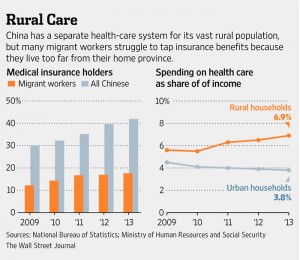
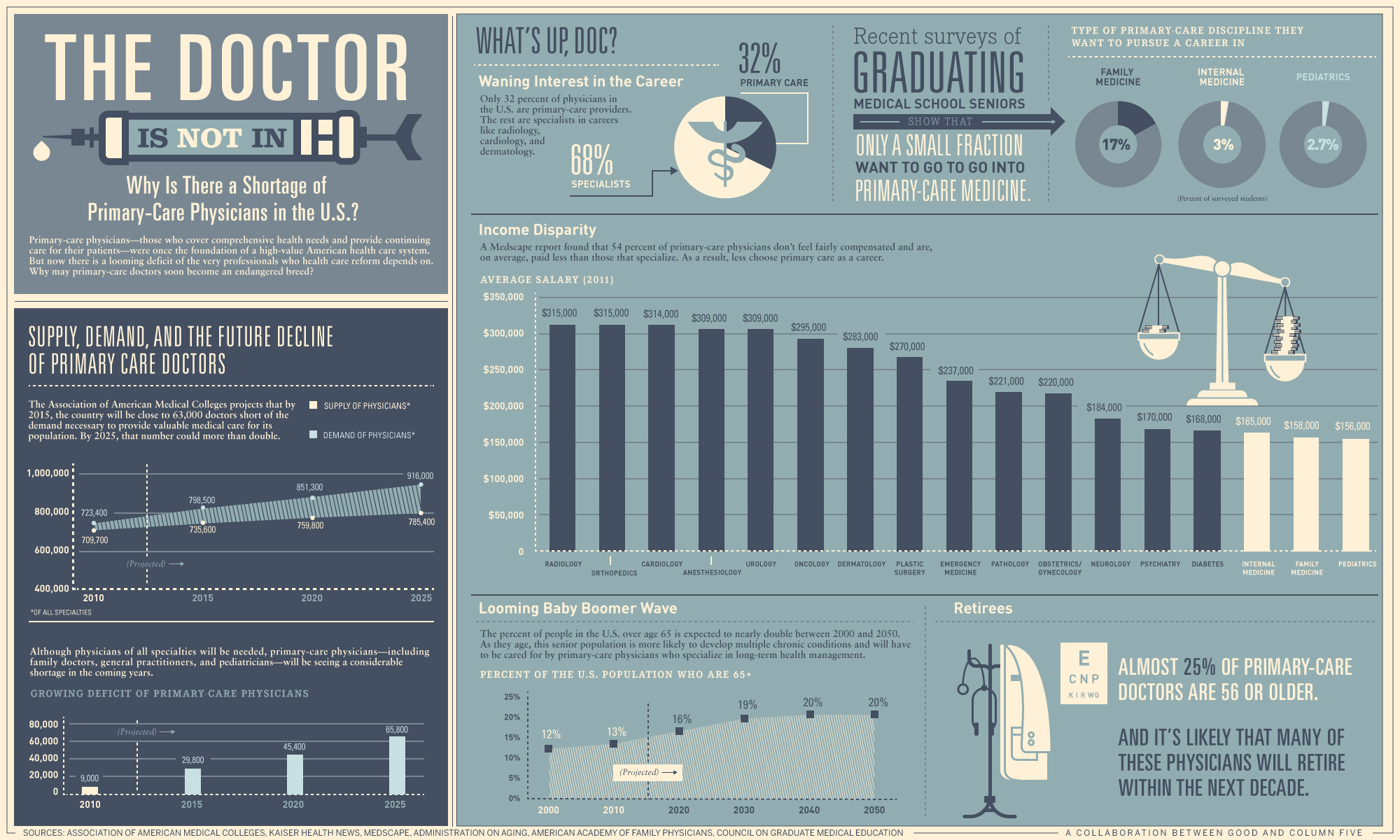 The US health care system is less centralized and has slightly different problems. First, there is a
The US health care system is less centralized and has slightly different problems. First, there is a 



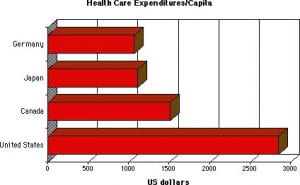


 According to the United States
According to the United States 


 regulations to cap or to reform the way insurance companies charge and calculate their fees. Federal and local regulations are not coordinated well in supporting and monitoring the quality, cost, and effectiveness of health services.
regulations to cap or to reform the way insurance companies charge and calculate their fees. Federal and local regulations are not coordinated well in supporting and monitoring the quality, cost, and effectiveness of health services.