 Around the world, many people have become isolated due to COVID-19 restrictions. During the pandemic, we have socially-distanced from those we love – with many people not seeing close family and friends for over a year – stayed-at home, socialized less, and have consigned to talking to people primarily through electronic devices. I appreciate platforms like Microsoft Teams and Zoom that allow me to stay in touch with people, but to be honest, I miss being around people in-person. Hugs. Handshakes. Feeling socially connected. I miss the
Around the world, many people have become isolated due to COVID-19 restrictions. During the pandemic, we have socially-distanced from those we love – with many people not seeing close family and friends for over a year – stayed-at home, socialized less, and have consigned to talking to people primarily through electronic devices. I appreciate platforms like Microsoft Teams and Zoom that allow me to stay in touch with people, but to be honest, I miss being around people in-person. Hugs. Handshakes. Feeling socially connected. I miss the spontaneous lunches with co-workers where we caught-up on our favorite television shows. Have you stopped to examine how this has affected your mental health over the past year? Have you been sad, depressed, anxious or lonely? I have! I have felt isolated due to isolation! However, when I think about this in the global context, I am thankful, and realize how privileged we are, because unlike many around the world I have technology to allow me to still interact with others and an Employee Assistance Program (EAP) that pays for mental health
spontaneous lunches with co-workers where we caught-up on our favorite television shows. Have you stopped to examine how this has affected your mental health over the past year? Have you been sad, depressed, anxious or lonely? I have! I have felt isolated due to isolation! However, when I think about this in the global context, I am thankful, and realize how privileged we are, because unlike many around the world I have technology to allow me to still interact with others and an Employee Assistance Program (EAP) that pays for mental health services. For many around the world this is not the case and I can’t imagine how truly isolating this pandemic has been for them. Can you imagine living in a remote village with no technology to stay in contact with loved ones or access to mental health services? For myself and others, the pandemic has highlighted the importance of investing in innovative global mental health initiatives and technology.
services. For many around the world this is not the case and I can’t imagine how truly isolating this pandemic has been for them. Can you imagine living in a remote village with no technology to stay in contact with loved ones or access to mental health services? For myself and others, the pandemic has highlighted the importance of investing in innovative global mental health initiatives and technology.
Suicide in the Global Context
 Suicide is a public health concern. Around the world, approximately 800,000 people lose their life to suicide each year. In 2016, suicide accounted for 1.4% of all global deaths, making it the 18th cause of death (Reference). Suicide knows no boundaries and cuts across race, ethnicity, sociodemographic level and all regions of the world. A suicide attempt is a crucial risk factor for subsequent suicide. Silence and stigma prevent those in need from seeking help. During the COVID-19 pandemic shelter-in-place policies and stay-at-home orders may increase the number of unrecognized suicide attempts or suicide attempts resulting in loss of life due to an individual being alone for a longer period of time before someone intervenes.
Suicide is a public health concern. Around the world, approximately 800,000 people lose their life to suicide each year. In 2016, suicide accounted for 1.4% of all global deaths, making it the 18th cause of death (Reference). Suicide knows no boundaries and cuts across race, ethnicity, sociodemographic level and all regions of the world. A suicide attempt is a crucial risk factor for subsequent suicide. Silence and stigma prevent those in need from seeking help. During the COVID-19 pandemic shelter-in-place policies and stay-at-home orders may increase the number of unrecognized suicide attempts or suicide attempts resulting in loss of life due to an individual being alone for a longer period of time before someone intervenes.
 Globally, suicide remains the second leading cause of death in 15-29-year-olds (Reference), after road injury, and the second leading cause of death for females aged 15-29 years, after maternal conditions. In males of the same age, suicide was the third-leading cause of death, after road injury and interpersonal violence. However, more men died from suicide than women with 13.7 deaths per 100,000 compared to 7.5 deaths per 100,00, respectively (Reference). The only countries where the suicide rate was estimated to be higher in women than men were Bangladesh, China, Lesotho, Morocco, and Myanmar.
Globally, suicide remains the second leading cause of death in 15-29-year-olds (Reference), after road injury, and the second leading cause of death for females aged 15-29 years, after maternal conditions. In males of the same age, suicide was the third-leading cause of death, after road injury and interpersonal violence. However, more men died from suicide than women with 13.7 deaths per 100,000 compared to 7.5 deaths per 100,00, respectively (Reference). The only countries where the suicide rate was estimated to be higher in women than men were Bangladesh, China, Lesotho, Morocco, and Myanmar.
Most suicides (79%) occur in low- and middle-income countries (Reference), where resources for identification and management are scarce; however, high-income countries have the highest rate of suicide at 11.5 per 100,000 population. Nearly three times as many men as women die by suicide in high-income countries, in contrast to low- and middle-income countries, where the rate is more equal.
Suicide Rates during COVID-19
 Currently, there is limited data on suicide rates during the COVID-19 pandemic or associated factors. However, as many countries implemented shelter-in-place policies and stay-at-home orders, many healthcare professionals were concerned for a potential increase in suicide rates, attempts, and ideation. Previous infectious disease-related public health emergencies, such as SARS and Ebola, have been associated with an increase in suicide rates and suicide attempts. There is evidence of increased suicide rates among older adults during SARS and in the year following the epidemic (possibly motivated by social disconnectedness, fears of virus infection, and concern about burdening others) and associations between SARS and Ebola exposure and increased suicide attempts (Reference). Additionally, several factors, which I talk about below, reinforce these concerns.
Currently, there is limited data on suicide rates during the COVID-19 pandemic or associated factors. However, as many countries implemented shelter-in-place policies and stay-at-home orders, many healthcare professionals were concerned for a potential increase in suicide rates, attempts, and ideation. Previous infectious disease-related public health emergencies, such as SARS and Ebola, have been associated with an increase in suicide rates and suicide attempts. There is evidence of increased suicide rates among older adults during SARS and in the year following the epidemic (possibly motivated by social disconnectedness, fears of virus infection, and concern about burdening others) and associations between SARS and Ebola exposure and increased suicide attempts (Reference). Additionally, several factors, which I talk about below, reinforce these concerns.
 Widely reported studies modelling the effect of the Covid-19 pandemic on suicide rates predicts increases ranging from 1% to 145%, (Reference) largely reflecting variation in underlying assumptions. A particular emphasis has been placed on the effect of the pandemic on children and young people, who based on WHO’s previous statistics, are most at risk for suicide. Numerous surveys have highlighted that their mental health has been disproportionately affected, relative to older adults, (Reference) (Reference) and some suggest an increase in suicidal thoughts and self-harm. (Reference)
Widely reported studies modelling the effect of the Covid-19 pandemic on suicide rates predicts increases ranging from 1% to 145%, (Reference) largely reflecting variation in underlying assumptions. A particular emphasis has been placed on the effect of the pandemic on children and young people, who based on WHO’s previous statistics, are most at risk for suicide. Numerous surveys have highlighted that their mental health has been disproportionately affected, relative to older adults, (Reference) (Reference) and some suggest an increase in suicidal thoughts and self-harm. (Reference)
Specific COVID-19 Threats to Suicide Risk
 Addressing global suicide rates during the COVID-19 pandemic will require considering specific suicide risk factors (e.g. increased social isolation, personal and economic losses), but also pre-pandemic risk factors (e.g. the increasing service gap between mental health needs and effective health care). Importantly, these factors may interact in previously unexplored ways. For example, an established suicide risk factor (e.g., access to lethal means) has increased during the pandemic. (Reference)
Addressing global suicide rates during the COVID-19 pandemic will require considering specific suicide risk factors (e.g. increased social isolation, personal and economic losses), but also pre-pandemic risk factors (e.g. the increasing service gap between mental health needs and effective health care). Importantly, these factors may interact in previously unexplored ways. For example, an established suicide risk factor (e.g., access to lethal means) has increased during the pandemic. (Reference)
Based on the growing body of science informing our understanding of suicide, there are several risk factors linked to the pandemic and ensuing public health measures, which suicide expert consensus views as threats that could lead to an increase in suicide rates if the proper mitigation steps are not employed. These threats to population suicide risk include the pandemic’s potential to lead to deterioration in mental and/or physical health; social disconnectedness, loneliness, or diminished social support; fears about or realized job or financial losses; remote work or school and the related disruption in social, academic, and basic structure to daily life; loss of loved ones or anticipated milestones; increased alcohol consumption in some regions of the world; and increased availability of lethal means such as firearms, opioids, and other toxic substances, especially with more time spent at home sheltering in place. (Reference)
deterioration in mental and/or physical health; social disconnectedness, loneliness, or diminished social support; fears about or realized job or financial losses; remote work or school and the related disruption in social, academic, and basic structure to daily life; loss of loved ones or anticipated milestones; increased alcohol consumption in some regions of the world; and increased availability of lethal means such as firearms, opioids, and other toxic substances, especially with more time spent at home sheltering in place. (Reference)
Beyond COVID-19: Suicide Intervention Programs
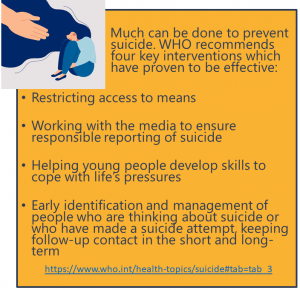
Currently, only 38 countries have national suicide prevention strategies. As the COVID-19 pandemic continues and countries plan to address the mental health effects, it is imperative for countries to develop innovative prevention strategies to address suicide rates-specifically in women and youth. Suicide prevention strategies should be intersectional and include plans to address stressors that could lead to poor mental health (e.g. unemployment, food insecurity, etc.) The World Health Organization offers guidance on national suicide prevention strategies.
References
Information in the Nepal Graphic (Reference)
Information in the Japan Graphic (Reference)
Information in the Japan Graphic (video)


There are no comments yet...Kick things off by filling out the form below.