Learning about Global Health has been an enriching experience. It has allowed me, and I am sure my classmates as well, to gain insight on issues and even solutions that other countries experience. The Global Health course has widened our perspectives as future public health professionals. Though the Covid-19 pandemic has altered the way the course is normally taught, effective teaching was still accomplished with the current course structure and activities. The readings, class discussions, and content materials we engaged with have all helped to cultivate a great learning environment. However there are other technologies and tools that can be integrated into the course to enhance the learning experience, especially during this mass transition to virtual living. Many people are working virtually from home, enrolled in school virtually, and visiting their healthcare providers virtually. Implementing a virtual reality component in courses such as global health could serve as an educational benefit for students by helping them achieve a much more substantial learning experience. It would help create a meaningful distance learning atmosphere by allowing students and our course instructors to be in the same room instead of our now normal Zoom and/or WebEx calls.

Virtual reality can be utilized to increase student’s learning and engagement by transforming the way their educational content is normally delivered. Textbooks, supplementary readings, contextually relevant videos, class discussions, lectures, and even guest speakers have been used in the past to curate an efficient classroom environment that promotes genuine learning. Virtual reality technologies can catalyze these efforts by creating a virtual world that allows students to see the content material they’re currently learning and also interact with it. Most people learn best by doing, so being able to “physically” engage with the environments they’re learning about would solidify their content retention by enabling emotional reactions to be created which will allow them to better remember what they are learning due to the experiences being meaningful and memorable. I don’t have any personal experience with virtual reality games, but I have witnessed other people use them and it is amazing at how engulfed they become with the world or activities they are participating in. It’s as if they forget that what they are currently experiencing isn’t reality because their bodies are under the belief that it is genuinely in a new place both physically and mentally. Translating these experiences into a classroom setting will allow students to learn new subjects by equipping them with the opportunity to virtually live it.
Depending on the activity, kinesthetic learners such as myself can unintentionally direct more of their attention on grasping the instructions instead of fulfilling them. Including virtual reality in educational settings can provide a supplemental experience anchor to the instructions so that students are motivated to discover for themselves by having the opportunity to learn by doing rather than just reading or watching educational videos. Visual learners would also benefit from virtual reality teachings because their access to visual aids wouldn’t be limited to just book illustrations or content supportive videos, they would be able to explore the topics and gain a better understanding of them.

Virtual reality would also benefit students by broadening exposure to different career paths. Public Health is such a diverse field. There are so many paths one could take with an MPH degree. This aspect of virtual reality could be particularly useful for MPH students by enriching our professional development with field work experiences that appeal to us. Regarding the Global Health course specifically, it could also provide students with field work in the countries and communities we learn about. Students would be able to gain firsthand experience assessing the global health issues we discuss and even collaborating with community members to develop effective solutions. Tapping in to our public health career interests would be extremely feasible. For example, MPH students interested in program planning could use virtual reality as an opportunity to do so. Some universities are already experimenting with virtual reality learning such as the University of Westminster. Their law students have used virtual reality technologies to hunt for clues to develop a murder case rather than compiling a case the usual way by reading witness statements. They were afforded the opportunity to walk around a building and form judgments on if someone would have been able to witness the committed crime. MPH professors could use this teaching mechanism to employ students with hands on experience creating, implementing, and evaluating interventions for the public health issues taught in their courses.
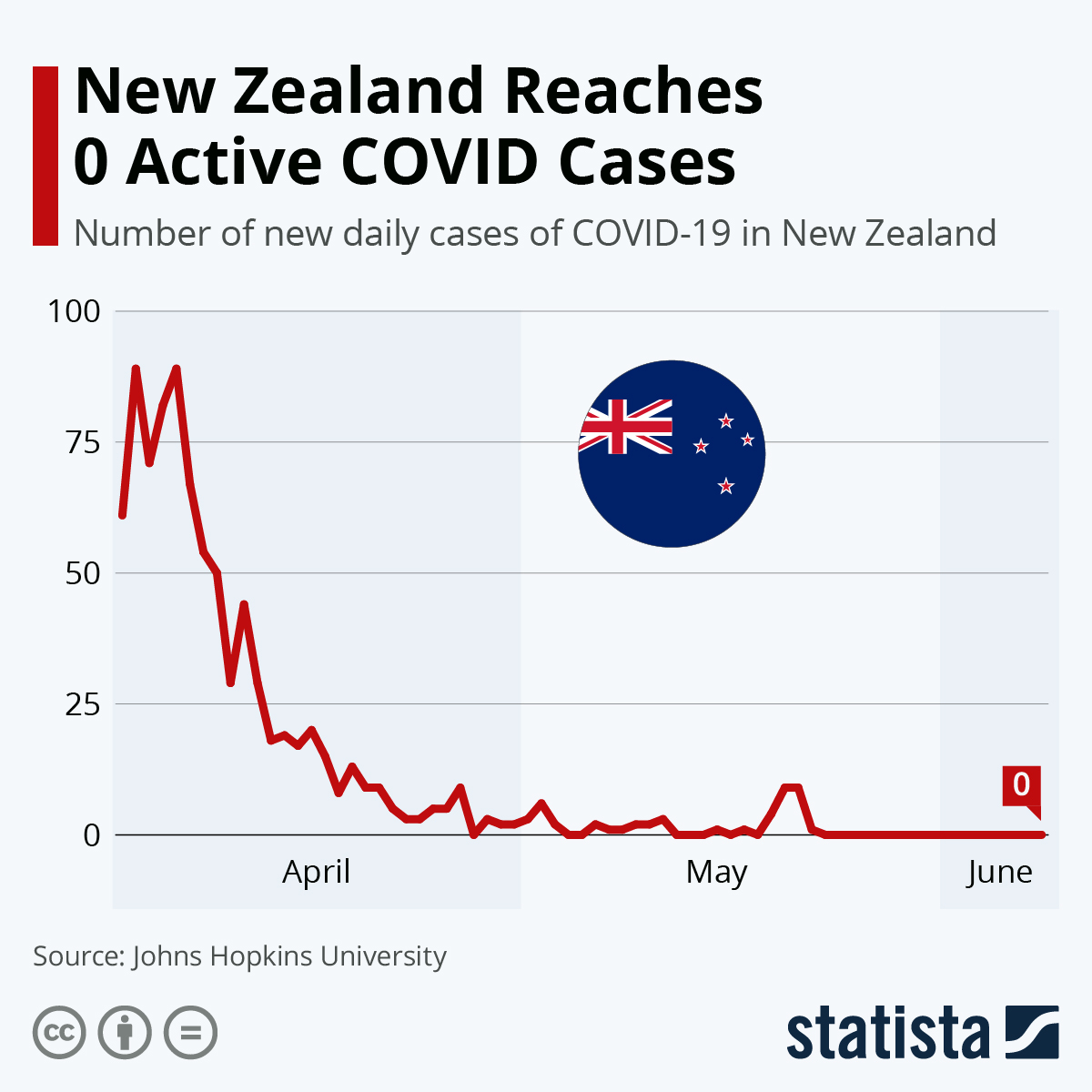
Google Expeditions is an app that features a library of virtual reality “field trips”. Some of the included field trips allow students to travel back in time. MPH students would find monumental educational benefits utilizing this feature of the app. In the Foundations of Public Health course, we could travel back in time to the very first public health/epidemiology intervention conducted by the “Father of Epidemiology”, John Snow. In the Global Health course, we could time travel back to the very beginning of the COVID-19 outbreak and collaborate on ways to effectively reduce, and maybe even eliminate, the spread of the virus. If widely implemented in school systems, this feature would be groundbreaking for students learning capabilities. Instead of discussing history, we would be able to witness and engage with it ourselves.
Lastly, virtual reality can provide social connectedness for students which is especially important today. Our new normal consists of staying isolated inside our homes to protect ourselves from catching this misunderstood, ever-changing virus. It would also enable student’s empathy and cultural competence by taking them outside of their usual classroom experience and allowing them to gain a concrete understanding of people’s unique circumstances across the world. This is of special importance and relevance today due to our current situations. Injustices across the nation, and the globe, continue to happen despite the pandemic we still have yet to overcome. Empowering students with these opportunities to learn about cultures, economic statuses, and accessibility experiences to vital resources such as education and healthcare outside of their own will shape them into becoming advocates for social, racial, and economical change.